Things I’ve Learned Recently:
1 in 38 people in the United States currently have Covid.
Azelastine, the ingredient in an over-the-counter antihistamine spray, may reduce contraction of Covid and rhinovirus (according to a new German study).
The very idea of another person wearing a mask makes so many people mad.
There is such a thing as too many nerve blocks over too brief a timespan.
For me, the number was probably 15 over 8 days.
Stopping when you hit that point requires having a doctor who appropriately weighs the significance of your reported symptoms of fatigue and diminished functional capacity.1
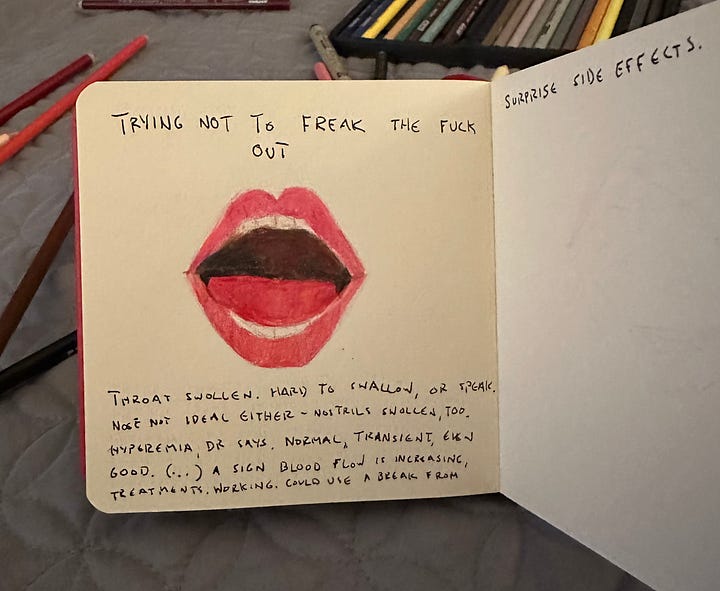
If you have trouble swallowing, breathing, speaking, and coughing, go to the Emergency Room.
If you develop the above symptoms an hour after having both sides of your neck shot up with anesthesia for the 16th and 17th time in 9 days, that’s probably the cause.2
If your doctor asks you to open your mouth over FaceTime and pronounces you fine, you should still probably go to the Emergency Room.
If your doctor says you’ll feel better in thirty minutes but later tells your father the symptoms could take 6-8 hours to resolve and that he neither told you this nor warned you of the potential side effect in advance because he didn’t want you to panic, it’s reasonable to consider that a red flag.
If the symptoms resolve by the following day, that’s great, but it’s not a green light to repeat the procedure.
If your doctor says you are the most sensitive Long Covid patient he has ever treated and, when asked to clarify whether he means physiologically or emotionally, he answers “Both,”….and/or if he regularly uses the word “anxiety” in reference to you…and/or responds to any and all symptoms you report or medical questions you ask with “It’s going to be okay,” he is probably undervaluing your physical symptoms.
If you accuse him of sexism and he says “fine, fine,” and tries to change the conversation, things are not fine.
If you have an even harder time breathing and speaking again the following day, after nerve blocks #19 and #20, GO TO THE EMERGENCY ROOM.
If the doctor tells you to come to his office instead and when you do, you find that he seems panicked and uncertain about what’s going on or what he can do, anxiety is a perfectly reasonable reaction on your part.
If your doctor is the country’s undisputed expert on sympathetic nerve blocks and the only person who has experimented with such an intensive protocol, anxiety is more than reasonable; it’s inevitable.
The subsequent crash WILL NOT be fixed by ANOTHER needle of anesthesia to the neck, no matter what the doctor says or hopes.
That 21st needle to the neck will, however, cause a reaction reminiscent of your adverse response to Reglan. Mercifully, Benadryl will calm the acute symptoms.
When you report said reaction to the doctor and, rather than presuming the cause to be the bupivacaine he just injected into two places on the left side of your neck, he asks, “Could it be a panic attack or your menses?,” though it will strike you even in the moment as too on the nose, that might be a good thing because it leaves no room for doubt: you’re done here.
What next?
I’ve been waiting until I felt better - or at least clearer - to write.
I do feel better than I did two weeks ago - for example, I can speak now - but that speaking constitutes an improvement underscores how off the rails things went.
The plan was always to do a certain number of nerve blocks over a period of days to be determined based on how I reacted to the blocks. Theoretically, though the blocks might worsen my fatigue initially, there would be a turnaround point after which I would see my baseline gradually improve, and we would continue the procedures until I hit a plateau.
Then, I would spend the next 6-8 weeks convalescing, in as restful and stress-free a state and environment as possible. Even if I felt better, I should be careful to curtail my activity and stress in order to give my nervous system time to rewire itself in a lasting way. I should also avoid getting sick, because that would ruin everything.
I should be resting now.
Writing this is not as strenuous as, say, walking around the block would be for me, but it’s probably more exertion than is advisable right now. Still, I’ve felt, and am giving in to, a nagging itch to write something about what’s happened, even if not a deep dive, to update everyone who has been following my journey, and to plant a tiny flag in the expanse of the internet in case there’s someone with an illness similar to mine searching for experimental treatments or considering doing a shit ton of nerve blocks over a short period of time.
Every body is different and hopefully what happened to me won’t happen to you. Apparently it hasn’t happened to anyone else my doctor has treated. But if it does, know that you’re not alone…And if it has, please let me know so *I* know that *I’m* not alone.
It’s distressing to find yourself in a situation for which you can find no relevant comparisons, no alternative experts to consult.
Hard as it is to believe - because isn’t there info about everything on the internet? – there really isn’t any information about the situation I’m in.
In the end, I received 21 sympathetic nerve blocks over a period of 13 days, with only one day off.
These numbers probably sound vaguely like a lot, but a little more context is probably necessary to emphasize the extremity of it. Almost nobody receives this quantity of nerve blocks period, and certainly not over such a short span of time. The scant existing literature about adverse reactions to sympathetic nerve blocks in general refer to a patient’s reaction to a singular or bilateral stellate ganglion block.3
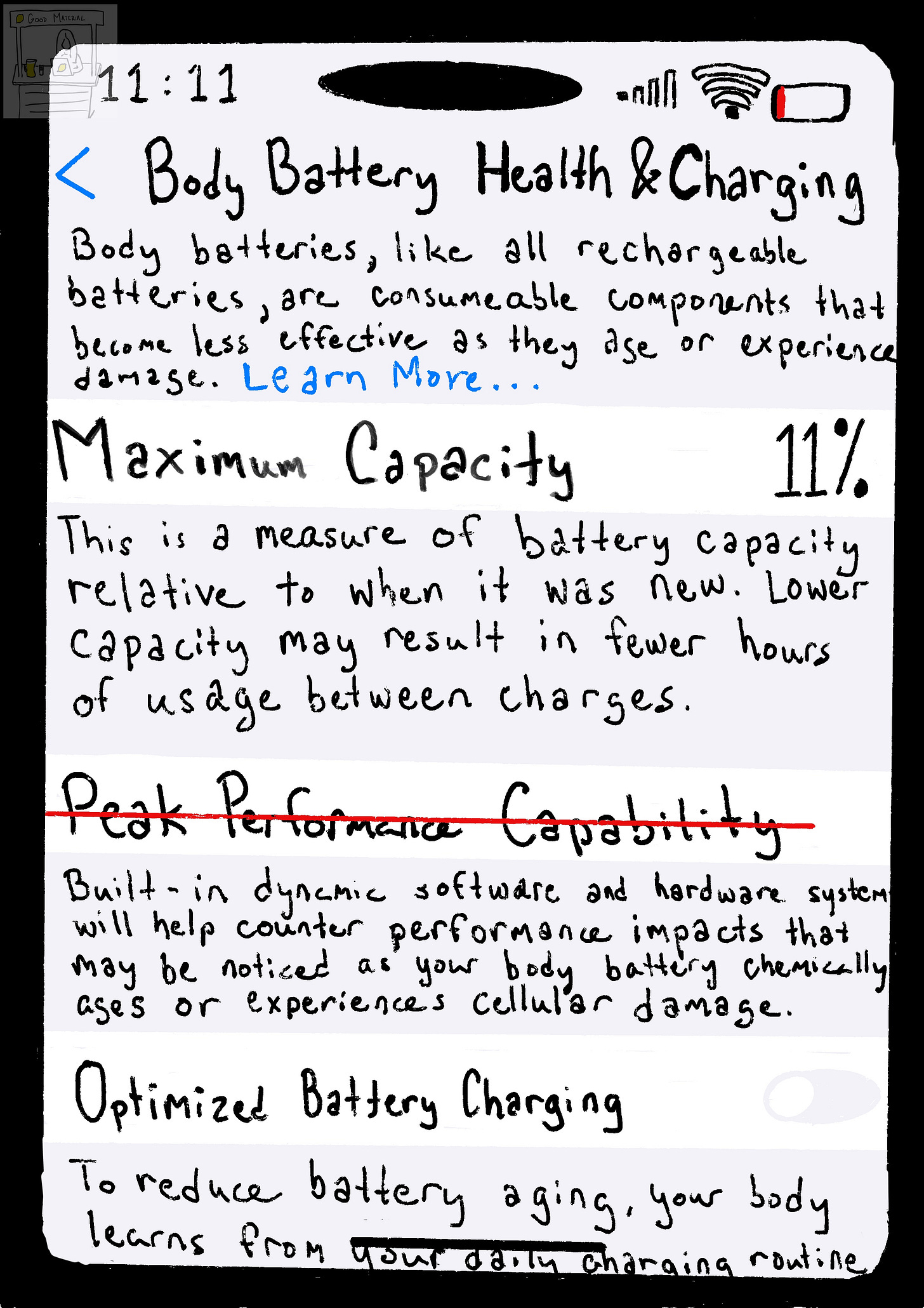
Before these treatments, I had better than average lung capacity. I’m a certified freediver. I can - or used to be able to - hold my breath for multiple minutes. I used to be able to hold my breath while diving down to 70 feet. Now, according to the incentive spirometer a nurse gave me when I finally, belatedly went to the ER, I have half the lung capacity of a healthy person my age. My dad, who has a frozen hemi-diaphragm, can breathe twice as deeply as me. Speaking at length is tiring in a way it never used to be. I have always had a voice that tends towards hoarseness, but it’s much worse now. I used to speak too loudly accidentally, now it takes effort to raise my voice. I have also developed new sensitivities to light and sound.
I have to believe all this is temporary.
The temporary result of too much stress on my system and a shit-ton of anesthesia spreading throughout my upper body in ways that the doctor couldn’t track or control, of anesthesia that maybe didn’t clear my body as quickly as it “should” have, which would make sense because my body processes everything slowly these days.
And so I am going to try my best to complete the program - to spend 6-8 weeks recovering from the stress of the past 3 and hoping that once I make it past the acute physical trauma, my nervous system might still rewire itself into a more functional state.
Maybe the nerve blocks will prove helpful in the end.
If they do, I will know that advocating for myself and my limits is what halted the treatments before they caused irreversible harm.
That will be a more empowering story than one that mostly lionizes a man with a magic needle. Although, if I do get better in the next two months, I will happily give him the credit he deserves.
As he has repeated to me multiple times over the past weeks, “I’m only a man, not a demi-god.”
I deeply hope he’s a man who will have - in his way, to the best of his ability - helped me, in spite of it all.

When I am experiencing severe symptoms, no matter how severe, if required, I can articulate how I’m feeling in precise detail. This capacity has turned out to be a double-edged sword. It seems to suggest that I have higher baseline functionality than I do. It doesn’t make sense, right? That I can write a two thousand word essay more easily than I can shower or brush my teeth twice a day? This is somehow impossible to convey in a believable way, even when I literally state it like that. Because if you don’t have ME/CFS, it’s hard to conceive of how punishing normal activities of daily living can be. Of how it feels to lie in bed and want to reach out for a glass of water but need to wait and work up the energy necessary to extend your arm, lift the glass, and then move your upper body into a position conducive to drinking.
Maybe my verbal facility enhanced the doctor’s perception that my sensitivities were as emotional as they were physiological. Or maybe it was merely gender – though that seems hard to believe, since most ME/CFS and Long Covid patients are female.
There was a day during my first week of treatment when the doctor saw me smile at something someone said and asked if he could take my picture. He had shown me before and after photos and videos of other patients - videos of remarkable transformations, stutters suddenly eliminated.
I assumed he wanted my photo for similar purposes.
What could I have said? “Yes, you can take my picture but please understand I can smile like this on demand, it is socially conditioned in me and has limited bearing on how I feel inside?” I guess I could have said that. But it didn’t seem worth it. I let him take my picture.
A sympathetic nerve block = a needle full of anesthesia injected into a nerve cluster connected to the sympathetic nervous system (that’s the “fight or flight” one). The parasympathetic nervous system is the “rest and digest” one. Both are part of the autonomic nervous system, which controls all the bodily functions operating outside our conscious control, from heart rate to blood flow to sweating to breathing.
Most of the nerve blocks I received were stellate ganglion blocks (SGBs). Those nerve clusters are located on either side of the neck.
Sympathetic nerve blocks temporarily turn the fight or flight part ‘off’ through the use of targeted anesthetic injected into a nerve cluster associated with the sympathetic nervous system. The idea is that when the anesthesia wears off and those nerves come back online, the system will reset to a more functional state. The blocks also increase blood perfusion, and stellate ganglion blocks, which are in the neck, are particularly effective at addressing neural inflammation, which is thought to be a significant problem for people with Long Covid.
Most people who do this treatment receive one, on one side of their neck, or two — a bilateral block. Usually the sides are performed on different days, or, if on the same day, with at least a few hours in between. If the treatment improves their symptoms, they might repeat the procedure again in several months.
Nerve blocks are most commonly used to treat chronic pain. Using them to treat chronic illnesses like Long Covid, ME/CFS, POTS, and MCAS is new. Among published studies, the most intensive protocol is a three week protocol of one bilateral block per week, each side administered on subsequent days. The doctor I traveled to be treated by created that protocol. When he said that, given my history and symptoms, he thought I needed something more intensive than the three-week protocol - and that he’s had great, and faster, success treating patients much more aggressively, and that - I said ok. I said yes, please. Stacking the treatments close together gives them a greater chance of efficacy — an experience I know to be true from ketamine treatment for depression. The more deeply ingrained your dysfunctional state, the more aggressively you need to break those signaling patterns. And repetitively, since the anesthesia is short-acting.
I received two blocks almost every single day of treatment.
The majority of the blocks I received were SGBS, but I also received four thoracic blocks, a celiac plexus block, and a bilateral lumbar sympathetic block. (I.E. needles full of anesthesia were injected into nerve clusters located progressively lower down my back, in order to improve circulation and function in my chest, GI tract, and legs.) The celiac plexus and lumbar sympathetic blocks were a level way up in intensity - both were performed in x-ray rooms with the assistance of a team in heavy lead vests. I started referring to the nerve blocks as procedures instead of as treatments after that. Treatment seemed too light a term. There is no published research on the use of these nerve blocks to treat my illnesses.



I so appreciate your writing, Izzy, but I’m so sorry you have to write about the extraordinary agony you’ve had to endure.
Just in case you hadn’t seen this a fellow novelist has penned a book about the MECFS scandal (despite the fact that like us, she can’t read a print book!). She has written some amazing stacks recently about the ‘mind body’ (psychosomatic) crowd determined to sidestep our need for medical treatment
https://longcovidadvocacy.substack.com/p/due-south-an-exciting-development?publication_id=1492584&post_id=173807338&triggerShare=true&isFreemail=true&r=293qwi&triedRedirect=true